Professor Soo Downe OBE:
The first time the story below was told, it was as a dramatic performance to the third international UK normal birth research conference in 2006. My intention in asking Kate and Sheena to do this was to highlight the fact that doing normal, out of hospital childbirth may end up exposing mother and midwife to litigation, because this choice is not seen as the standard, ‘safest’ option, despite evidence to the contrary. I was particularly keen for midwives to recognise the need to be courageous in facing this possible outcome. The argument was that facing our fear of litigation may reduce the risk of defensive practice: once the worst has been faced and accepted, there is nothing more to fear.
Kate’s part of the story illustrates the fact that, often, women are caught up in litigation in a way that can be as damaging as the original trauma suffered in unexpectedly pathological childbirth. No-one is a winner in this circumstance. Sheena and Kate show in stark and clear-sighted detail what this experience feels like, and how it is possible to work through it, overcome it, and still maintain faith in normal birth processes, and in mutually respectful relationships.
Mother meets midwife
They met on a winter’s morning in 1994. Kate was a 30 year old woman who had recently returned from four years living the East, working in refugee communities, with her Tibetan husband. Although she had grown up in Lancashire she was living in Swansea, South Wales, working full time in a hostel for homeless people, when she became pregnant with her first child in July 2004.
Sheena was a community midwife with experience of home birth and ten years in a GP maternity home (similar to a birth centre) where there was no medical cover.
For Kate choosing a home birth seemed quite normal: she was born at home, as were her siblings. Her mother is Dutch and so home did not seem so unusual. She had read up on the subject and had direct experience of how things can be in hospital. Kate had been by her younger sister’s side when she was taken for an emergency caesarean, the direct result of over intervention.
For Sheena home birth was the ultimate practice for the use of her midwifery skills. She had worked in the GP maternity home where there was no technology other than emergency life-saving equipment, and had seen the benefits that brought. More than this, her desire to assist women in their choice was and still is her passion.
Kate had received her antenatal care in another area, where she was booked for a home birth. She wasn’t given GP cover but the midwives were very supportive and discussed the home birth guidance and support with Kate. However Kate lived a house shared with two other men, both smokers, attached to the hostel where she worked. When a friend suggested that Kate move to a more beautiful peaceful area close to where her parents lived, to give birth and stay in the friend’s spare house, Kate wrote to the Head of Midwifery to explore the possibility of transferring the home birth option there. In the last month of the pregnancy Kate moved up to the Ribble Valley and met Sheena, the midwife who was going to provide her care. Sheena had been asked to care for Kate by her manager, who had read Kate’s letter out during a team meeting.
Our story
Kate: Sheena and I clicked right from the start. She was so open and respectful, and interested in me as a person. I trusted her and was delighted that she would be with me on this amazing journey into motherhood.
Sheena: I sat on the floor in Kate’s home and she offered me Tibetan tea. Kate told me her story of pregnancy so far, and her desire to birth at home. It was Kate’s first baby and she was so excited. I didn’t meet Cheophel her husband but heard all about him, and felt privileged and happy to be their midwife. I told Kate I would try to be available for the birth by being on call for the three-four weeks necessary.
Normal procedures were followed. There wasn’t much discussion about the choice of home delivery as the decision had been made in Wales and discussion had taken place there.
Kate: I didn’t think to ask lots of questions about travel time and distances to hospital: I assumed that if the midwives were happy to take me on, and had done the same for other women, it wasn’t an issue
Sheena: I didn’t go into any great detail about distance from hospital etc as I rightly or wrongly assumed Kate knew how far the hospital was. It wasn’t my practice to do so, as I had a worked in a maternity unit for ten years that was quite near to where Kate lived, and transfer hadn’t been a problem. Kate wanted a home birth, she was very healthy and happy, and ready to meet her baby.
Kate called Sheena the morning she went in to labour and she attended shortly afterwards. Kate’s labour was amazing; she was active and alert, calm and serene, and very excited. Cheophel and Lucy (Kate’s friend) were present, and providing wonderful support.
Sheena: I loved caring for Kate. I remember her movements, her smile, the lambs in the fields outside and the loving touches of her birth partners. She was agile, and worked with her labour like a strong, proud woman.
When there was spontaneous rupture of membranes, Sheena performed a vaginal examination to exclude cord prolapse (practice at the time). Kate was standing for the examination, and her cervix was found to be fully dilated. The head however, was still above the ischial spines, and Kate had no desire to push. The second midwife listened to the fetal heart, and there was acute prolonged bradycardia.
The emergency services were called……………
Kate: I had felt strong and centred, but now I started to feel powerless.
I knew things were not going as they should, but there seemed to be nothing I could do about it. I tried to remain calm, to not panic, to breathe deeply. It was my first child, so I had no experience to measure it against. I looked to Sheena for guidance; she my anchor. Time seemed to stretch out and slow down, I recall an incredible sense of clarity but huge waves of fear rising within that..
Sheena: The fetal heart beat was still 60bpm. Immediately my feelings lunged from fear, hope and an urgency to protect. The fear was the strongest sense, and increased with each passing second. I couldn’t do anything. Kate was mobile, so changing her position was a constant thing, and the baby couldn’t be born yet. When the baby’s heart beat increased slightly, hope returned but disappeared as quickly as it came. I knew emergency services had been called so in terms of ‘correct procedure’, all was in order. But it was not. Reality was the person in front of me, Kate, who trusted me implicitly and whom I couldn’t help. I will never forget Kate’s eyes, looking into mine, searching for something that I found so hard to give. I wanted to say; ‘it’s good Kate, you are going to be fine’ but I couldn’t because I wasn’t sure that it was. How could I lie to her. Words that have always come so easy to me during my career were now unsuitable and inappropriate. Neither could I say ‘I am sorry’, as I would have done had fetal death occurred, because the possible outcome couldn’t be spoken about. I had an incredible overwhelming desire to take Kate in my arms and make her safe, or to somehow speed up the birth. But I could neither.
The ambulance arrived 40 mins after the call to the hospital. A local GP was present, but couldn’t assist. The procedure at the time was still the ‘Flying Squad’, where an ambulance was called as an emergency, but it necessitated calling at the hospital to collect the necessary clinicians. The communication between the hospital and ambulance control initiated a response to send one ambulance with obstetrician, midwife, paediatrician and full resuscitation equipment. The room where Kate was small, and yet the paediatrician began to set up the equipment, and the doctor urgently proceeded to examine Kate.
Kate: The house seemed to have been invaded; people upstairs, downstairs, on the stairs, in every room; women and also men that I didn’t know, disembodied voices, glimpses of uniforms. The registrar examined me and didn’t inspire confidence or trust; she seemed authoritarian towards me, but scattered in herself. I looked to Sheena trying to keep the connection, trying to find the direction. My impression was that she had been blocked out by the registrar who had taken over control, and yet didn’t seem in control. It felt as if I had been cut loose, adrift on a sea of emotions I hadn’t been prepared to negotiate.
Sheena: The ambulance was here, and familiar faces. Fetal heart still 60. The doctor was experienced, the midwife a trusted colleague, the paediatrician and his equipment. An examination, questions asked, and a flurry of activity. The doctor wasn’t happy to try to deliver the baby, and asked for Kate’s transfer in. Another ambulance was needed, as Kate and the equipment could not fit in one ambulance. The baby could have been born during the journey. Despair increased and fear intensified. Doctor’s instructions. Confusion and uncertainty. Cheophel looked so afraid, yet I wondered if he really understood the seriousness of the events. How could I make him feel better? I couldn’t speak his language and even if I could, I was unable to say the right thing. I touch his arm but I can’t smile.
Kate asks ‘should I push?’ ‘No’ says the doctor, ‘baby’s position is not good, head too high’. I knew this was so, as I had examined Kate. Kate looks to me not the doctor. Eyes burning into mine. What could I do? Fetal heart still 60 bpm. Despair.
The second ambulance arrived, and transfer began a further 44 minutes later
Sheena: Some relief when 2nd ambulance arrived but only because something could progress. The fear was still strong, what was to be?
Kate: I started to feel annoyed with everyone else apart from Sheena; I just wanted them to go away and to get back to the birthing we had been dealing with together. I felt that I was no longer present as a person any more; that the whole birthing had been taken out of my hands. I was no longer a woman giving birth to a baby, but a body out of which a baby had to be extracted. I was both acutely aware of myself and at the same time felt entirely disconnected from myself. There was an almost tangible feeling of alienation, which I can only describe as an out of body experience as I observed all of those things happening to me but without my being involved. My body was led down the stairs, my nakedness barely concealed as I stepped out into the spring day on to the street.
The hospital is 12 miles away, and it is peak time. Transfer to hospital began to with the assistance of the blue light. Kate was with Choephel, doctor, Sheena and another midwife who came in 1st ambulance. The 2nd ambulance followed with paediatrician and equipment.
Choephel was sat at the bottom of the stretcher that held Kate. Sheena was stood close, trying to listen to the fetal heart. The other midwife recorded the activity. Kate wanted to push during the journey.
Sheena: The journey was so difficult for Kate. Fetal heart still 60. She was desperate and scared, and I could sense such sadness in Choephel who I knew understood the level of urgency. When Kate wanted to push, I could see the baby’s head advancing Lots of black hair. From his position, Cheophel could see too, and looked at me for a solution. As I would normally do, I encouraged Kate to push and to ‘go with her body’. The doctor intervened and told Kate not to push as the hospital was in sight. She (the doctor) didn’t want the baby born at the roadside. Kate found this hard and looked at me for guidance. I felt it appropriate to continue to tell Kate to do as she felt necessary and to push if she wanted to.
Kate: It didn’t help that I was being given conflicting advice-don’t push-push. I felt intense anger (often associated with transition). Who was holding me? How long would I continue freefalling?
Pema was born on April 12th 1995, a full term baby weighing 7lb 8oz. It was a vaginal birth with an episiotomy.
Kate: She was blue, she seemed big and strong. Cheophel told me that she looked dead and he burst into tears. I was just so relieved that she was out, and alive; that was it, we did it, the baby is born end struggle, I thought. I didn’t realise that the struggle had only just begun.
Sheena: We arrived in hospital and Pema was born immediately. Her condition was poor and she went to NICU. This was the worst experience of my career. In bed that night I thought so much about Kate and Choephel and their sadness and worry. I didn’t sleep much and went through my actions, feeling sure that I had acted appropriately, although I remember wishing I had taken Kate in my car to hospital: an action worthy of instant dismal.
Two supervisors of midwives scrutinised my records and called for me the following day. The meeting was unnerving due to its formality, but my seniors assured me that there were no discrepancies with my care and that my record keeping was good. I visited Kate twice that day, and became part of the grief and concern that enveloped the whole family. Sometimes I wondered if my colleagues felt blame towards me as some didn’t really know the story. I also felt alienated by midwives who believed in 100% hospital birth system, as they said nothing to me. Not much support really.
Kate: I remembered meeting the doctor the next day by chance on the corridor. She enquired after ‘baby’ and then said to me ‘so next time you will be having baby in hospital yes?’ I was too socked to reply, but felt like slapping her.
Kate and Pema came back to their borrowed home after 3 weeks in Intensive Care.
Kate: We had not been in contact with hospital Social Workers. We had not been offered any counselling. We came home with drugs for Pema and a telephone number for SCOPE given by one of the nurses. I remember thinking at the time ‘’ SCOPE, that used to be the Spastics Society- why has he given me that?’’ The words cerebral palsy had not yet been used in connection with my baby. She was so beautiful and precious, our first born child, nearly lost to us. But as she gradually came off the phenobarbitone, a sedative which had kept the seizures under control, she began to scream. She screamed round the clock. She could not be put down even for a second, without hyper extending and screaming. She slept in 5 minutes snatches around and then only if she was being jogged about and bounced vigorously. Thus began a three year round the clock marathon. Our arms grew strong, but our spirits grew weak. We became exhausted. There was no let up. No involvement from Social Services, no respite care, no professional support apart from visits to the consultant for scans and check ups. More drugs were given to help Pema sleep. They were ineffective and that was when the epilepsy kicked in, leading to more drug, prescribed by trial and error.
Over the next year, no-one addressed the emotional side of what we had been through and continued to go through. We were expected to cope. Four lives could very easily have been lost at this point; Choephel tried to take his life, I seriously considered aborting my second child, and then taking my own life; and there were times when we had to leave Pema alone screaming just to prevent ourselves from harming her. We were just so tired. We couldn’t see a way forward. No-one knew how things were for us
Sheena: My work location had changed, but I stayed in touch with Kate and her family. My desperation continued, seeing the distress and despair of this young family. What could I do?
18 months after Pema was born Kate had another baby
Kate: There were medical reasons why I couldn’t go for a home birth this time, even though the system for transfer to hospital had changed. I requested permission for Sheena to be my midwife. I wanted to do it with her by my side again; I wanted it to be a shared experience which could help us both, and it was. I think it was at that point that I reconnected with my own inner strength.
Sheena: It was important for me to be asked by Kate to care for her when she was pregnant with her second child, and it gave me hope and confidence in myself as a midwife.
Some two and half years after Pema’s birth, Kate and her family were at a charity event for disabled children. A solicitor who was a personal friend of Jane the charity founder, was speaking at the event on the litigation process. After the talk Jane introduced me to the solicitor, told him the bare bones of Pema’s birth and suggested that he take a look at Pema’s birth circumstances to see whether he felt that there was any negligence on the part of the NHS Trust.
Kate: I went along with it; I felt that it would be quite clear cut.: either it would come out that they had messed up with the transfer to hospital, or it would be shown that everything was done properly. It seemed like a good idea to have someone ‘independent’ look at the facts. I was still very upset about things, used to burst into tears in shops, at meetings, whenever Pema was mentioned really. I suppose I was looking to the solicitor for a form of closure, and for support. But I was very naïve; I had no idea how litigation works, having no previous experience
Sheena: Kate and Choephel told me they had met a solicitor who was going to look into the birth of Pema. They respectfully asked me what I thought about this, and if I had any objections. They were clear they didn’t want to hurt me, and that they were totally happy with the care I gave. Their concern was in relation to the doctor and the transfer to hospital. I felt unclear about the litigation process, and was naive in my belief that as I had given good and appropriate care to Kate and Pema to the best of my knowledge and ability, I had nothing to fear. I gave them my blessing and said I would do anything to help them.
After some years there was a change in the litigation process
Kate: From the initial investigation the solicitor decided that there were strong grounds for a claim as there had been negligence during the transfer to hospital. This did not surprise me .I was asked to write an account of how I came to be giving birth at home and what happened just prior to labour, during labour and something of our life since then. It was very painful but I managed to detach myself from the process enough to write about it. Things took a long time, it was years, before we received any reports from witnesses and expert witnesses. From the expert witness reports there were new allegations which focused on the care of the midwives, which we had never been worried about. We were told that the case would now have to include all these new findings. After the statement which I sent in I was not asked to give my comments on any of the reports that came in; I was told that as Pema’s litigation friend I had a duty to accept the reports of experts I order to seek justice for her. My role in the process became very passive. It seemed to have a life of its own.
Sheena: The Trust’s solicitor emailed me to ask me to call her immediately. New allegations, this time challenging my care. She would send the account, but told me not to worry. I read them with horror when they arrived. My first thought….did Kate believe this? Wasn’t allowed to find out. Did she think I had cared for her inappropriately, without skill and judgment and that I had failed her? She signed to say she did. Oh God this can’t be true.
Anger towards the ‘expert’ midwife who wrote things about my care, that was good and provided with such passion.
Local press, two separate newspapers. Front page news, detailing names and allegations against Sheena. Kate was out of the country and unaware of the events unfolding. The papers were local to the town where Sheena was born and lived most of her life, and where she worked as a community midwife.
Sheena: My colleague had bought the paper on her way into work on a late shift. She brought it straight to me. Horror. It couldn’t really be happening. How can this be allowed when nothing was proven and no case heard? My name, my career, my reputation. What will the mothers of whom I have cared for over the many years think? I felt sure they would think… ‘lucky escape’ or liken me to Harold Shipman. This may seem ludicrous and far removed from reality. But reality for me. Need to leave my job. My children had comments at school. My neighbours quietly mentioning it to my husband at the bottom of the garden. Pointed fingers.
Kate: We returned from a very difficult but amazing trip to visit my husband’s family in Tibet; he hadn’t been back since leaving as a refugee 17 years earlier. I was pregnant with my 4th child. We were all ill and exhausted. We were fighting to get adaptations done in the home before my pregnancy advanced much further, so that I wouldn’t have to lift Pema so much. We were waiting for a date for major hip surgery for Pema whose left hip was fully dislocated. She was in constant pain and spent much of the time screaming. And to top it all we were presented with the front page newspaper article. Everyone we knew assumed that we had consented to the article. Everyone we knew assumed that what we were doing was taking Sheena to court. And without any knowledge of the facts everyone assumed that we were wrong.
A petition to the newspapers was circulating, saying that it was wrong to print these unproven accusations about Sheena. We agreed that it was wrong, but felt hurt that the petition didn’t say that it was also wrong to portray us as enemies of Sheena. We were following a legitimate legal process but were being treated as if we were the wrongdoers not the victims.
Comments form mums at schools, insults from people who had formerly supported us. Accusations that we were money grabbers. Support form no-one. Even close friends urged us to drop the case due to the damage it was doing to our family and to Sheena’s
Deep depression for the next few months. Isolation. Hated living in Clitheroe. Wishes for it to all be over, solicitor encouraging us to keep going and soon we would have the financial security to be able to move away
But things didn’t work out that way….
Kate: The Solicitor had only met me one time after that initial meeting. Now he came to visit us with the Barrister. I had made it clear that our concerns did not involve the midwives but of the emergency services. They explained that although negligence had been firmly established with regard to the transfer to hospital, causation had not, because It was difficult to prove that the delays caused by the negligence were the cause of brain damage. The expert witnesses were saying that Pema could have been born sooner, if transfer had been more efficient, but probably not less than 1 hour after the bradycardia. They would be using all the evidence including the evidence against the midwives to support the case, and as Pema’s litigation friend I had a duty to allow them to proceed. There had been an offer of a small out of court settlement which was less than the amount than they would be paying in court costs, so no risk. The solicitor warned me that if we didn’t go to court I would spend the rest of my life wondering what would have happened if we did.
I had just had a baby, I was very open ,quite emotional. I knew that I couldn’t stand up in court and pretend that I believed the midwives had to been to blame even if it was necessary to do so. I also knew that whatever part I played in the proceedings if the case was won on those grounds and not on the grounds of the mess up of the hospital transfer I would spend the rest of my life regretting it.
We telephoned the solicitor a few days later and asked to accept the out of court settlement and withdraw the case. The offer of a settlement was then withdrawn, and it had to go to appeal. Eventually we received an amount of money which has not changed Pema’s life much, except that we could buy her a wheelchair adapted van. We still live in the same place, we can’t afford to move. We still feel isolated, let down by the community. Unsupported. Outsiders. Pema the brave and the beautiful continues to be the epicentre of our lives.
Kate has her own perspective of how this system has failed her:
I believe in the right of a woman to birth in the place she feels is most appropriate for the type of birth experience she wants for her child and herself. The right to have unbiased information to make an informed choice, and support in the choice she makes.
I believe that birthing can be an amazing spiritual experience. I believe that intervention should be available for emergencies but that it should not be the norm, and sensitivity is one of the greatest attributes of a good midwife- when to help, how to support, when to hold back, when to do nothing, letting woman and child lead the way.
Pema’s birth was such a shock; nothing in my life could have prepared me for that experience. But I think that the shock waves which have coloured my whole life since then could have managed better, and I could have had support in integrating the experience, rather than being left with a huge open wound.
I have lived with anger just below the surface for years now. There has been no real closure of the events of the day that Pema was born. I had expected the litigation process to clear things up, and allow me to find the type of resolution that no-one else had allowed. Apart form the legal system no one was looking at Pema’s birth at all, not even from the point of view of how it affected us as a family, or me as a woman. But the legal process made things less clear, muddied the waters and confused me even more. I still had no resolution or closure, just new issues to deal with.
We were abandoned by the services that should have supported us. We were then taken on a desperate journey through the process of litigation which promised a way to escape from some of the problems we had been left with, but which ultimately only added to our problems. I feel that we should never have had to go through that process, and that justice is a game in which you have to play dirty if you want to win. We became pawns in that game, and it took a certain amount of moral courage to get out of it.
Although Sheena and I weren’t allowed to communicate during the whole process. I felt it important to send cards and letters to reassure Sheena that there was no personal animosity, no change in my feelings for her. Why did we have to be placed on opposite sides of this artificial fence? Discussion of the case with Sheena since it was closed has been the only thing that has really helped me to face what happened and come to terms with it, and start unravelling the threads of anger running through my life.
I was not free to choose the place of birth for my 3rd and 4th children, who were born without any intervention or medication and could have been born at home. There were too many issues, and it was clear I was not going to get support. I wasn’t going to do home birth as a battle: I had other battles to fight on Pema’s behalf.
I don’t regret my decision to enter into the process of litigation; what happened at Pema’s birth was swept under the carpet and litigation was the only choice on offer for me to face what happened so that I would be able to close that chapter. I do regret that there is no system in place in this country that can allow a family to honestly and openly request what happened in such circumstances as ours to be looked at, without the need for someone to blame; that there isn’t a supportive way to acknowledge events and their far reaching consequences, even accept shortcomings, provide redress, and enable us all to get on with our lives, integrating the experience however difficult. And while we struggle to support Pema, millions of pounds of public funds have been spent, both on the side of the NHS and through legal aid provided to Pema, most of this going into the private sector of solicitor firms. Would those millions not have been better spent supporting the damaged child?
I have no regrets about withdrawing from the court case; it was the only way for me to remain whole, and in my case I could see that the outcome would constitute neither justice, nor clarification, nor the closure I sought.
I do very much regret that the key players here, Sheena, Sheena’s family, myself; and my family, have had to go through so much heartache, and that my birth damaged daughter does not have what she needs to make the best of her difficult life.
Sheena also has her perspective as a midwife about how the system failed her, and how it should change:
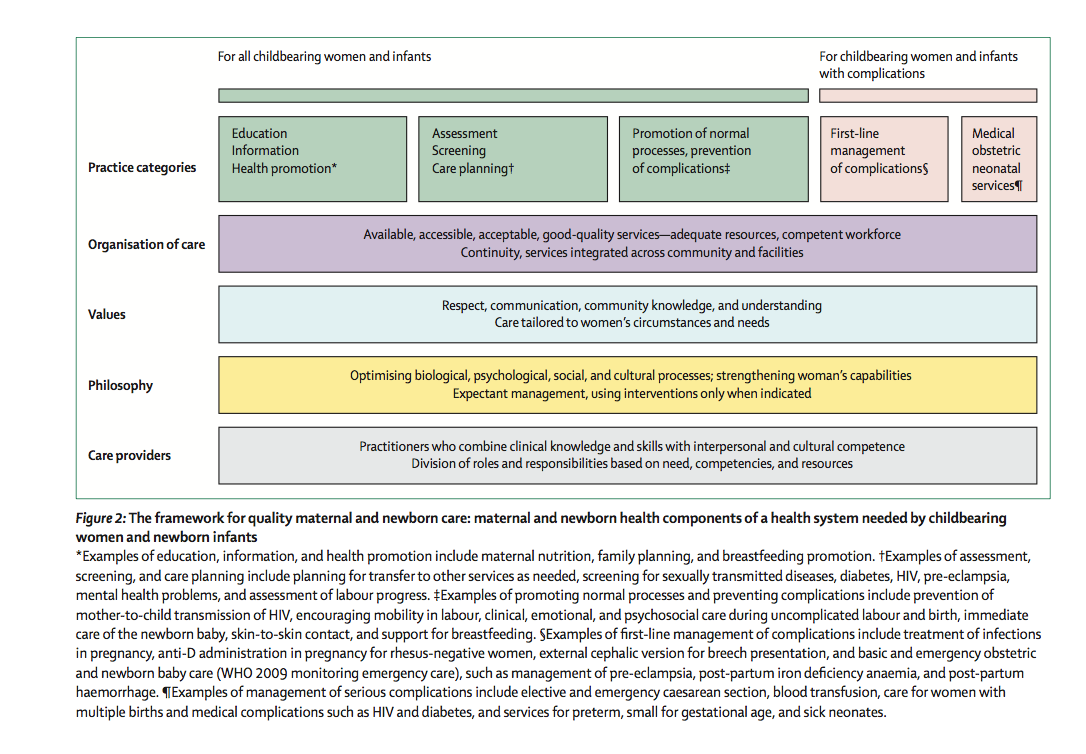
I believe in a woman’s ability to birth her baby, and that unbiased information should be offered to all women to help them choose their birth environment, with appropriate support for ultimate safety. Risks and benefits should include those in hospitals, as well as home.
Pema’s birth taught me that I can’t always make things right, and sometimes, no-one can. It has, however, destroyed part of me that believed and respected British systems, and it has borne in me disgust in the purpose and philosophy of the press.
I didn’t know how to act appropriately following Pema’s birth. Kate was too traumatised to discuss events in detail, and I was unsure of doing so. No discussions between senior medical teams or managers with Kate as to the sequence of events and how things could be better. This has now changed, and there would be dialogue with Kate and her family, and potentially more support.
Once the litigation process began, the destruction started, for me and for Kate. I wasn’t allowed to communicate with her at all, which became harder following the press incidence. I wanted to speak to her and to tell her the allegations were false and that my care was good, but couldn’t.
Since the closure of the case and we have discussed events at length, I feel betrayed by a system that wouldn’t let me care for Kate when she had her third and fourth babies. I would have cared for her at home if Kate desired.
What changes should take place? Sheena and Kate feel:
Sheena: In midwives training, students need to learn about the litigation processes and their effects, without the fear of blame.
Kate: Parents of damaged children need to know about what they could be letting themselves in for entering litigation, and perhaps a solicitor is not the best person to offer that advice.
Sheena: Health services to continue to commit to transparency and openness within their services, and acknowledge failure with an apology if appropriate.
Kate: There needs to be acknowledgment of the events and their emotional impact, the questions that arise-even the ones with uncomfortable or no easy answer. Different aspects will need addressing at different times, but without open acknowledgment this can’t happen. Litigation should not be the only way for this conversation to take place.
Sheena: Parents of babies born damaged or in need of long term care should receive immediate support, without the need for blame.
Kate: The birth of a damaged child should not require parents to turn into fierce warriors continuously fighting for support and services. Litigation should not provide the only way for families to guarantee that their child’s needs will be met.
Sheena: The media should be prohibited by law to publish details of health care professionals, unless they are a proven danger to the public.
It seems that women are loosing out in all of this, and that solicitors are the only ones to gain. And yet, due to our belief in each other and in spite of what has happened, we have travelled a full circle and are firmly back to together again, where we started.
Kate: I trust and respect Sheena as a midwife and friend and given the right circumstances I would have no hesitation in asking her to support me in delivering my baby at home. I would advise my own daughters that given the right circumstances, home is the best place to bring your child into the world.
Sheena: I still believe in home birth, and supported my daughter in her home birth choice recently. My philosophy is clear that women must do as they feel, and be given unbiased evidence based information to make their choice. Kate and her family are an important part of my life, and I will always feel privileged to be part of theirs.
So what next?
We were almost destroyed by this experience, for very little gain, and although we are back together, the litigation system continues to drive women and midwives apart.
In 2003, the government consulted on a document entitled Making Amends (DoH 2003), which set out proposals for reforming the approach to clinical negligence in the NHS. These ‘redress’ reforms however, have never been implemented.
In 2004/05 422 million was paid out in litigation costs, an example of how costs can run so high is that Kate’s case tool almost 8 years to complete, and her solicitor charged £100 against the case every time a phone cal was made to Kate. We feel that public money needs to be targeted where it is needed as opposed to lining the pockets of the legal profession. New Zealand, Scandinavian countries and France have introduced no fault schemes for medical injury, Virginia and Florida in America are introducing no fault compensation for babies with birth-related neurological injuries. The advantages of these systems are that lawyers are not routinely involved, reducing the amount of costs to legal profession and enabling more efficient targeting of resources.
Kate wanted to tell her story for clarity, to make sense of what happened, to assist in the integration of the experience. She feels it may promote a connection- with other women, midwives and mothers- to encourage them to have courage and to give insights into how the current system is failing women. Sheena feels the same, by telling her story she wants to strengthen professional courage and belief in women and midwives as true partners.

Chapter from Byrom S, Murry K (2009) In: Walsh D, Byrom S Birth Stories for the Soul Quay Books, London
Reference
Department of Health (2003) Making Amends: A consultation paper setting out proposals for reforming the approach to clinical negligence in the NHS London